FAQ’s acute encephalopathy and delirium
- Knowledge Base
- FAQ's Acute encephalopathy and Delirium

Acute encephalopathy and delirium
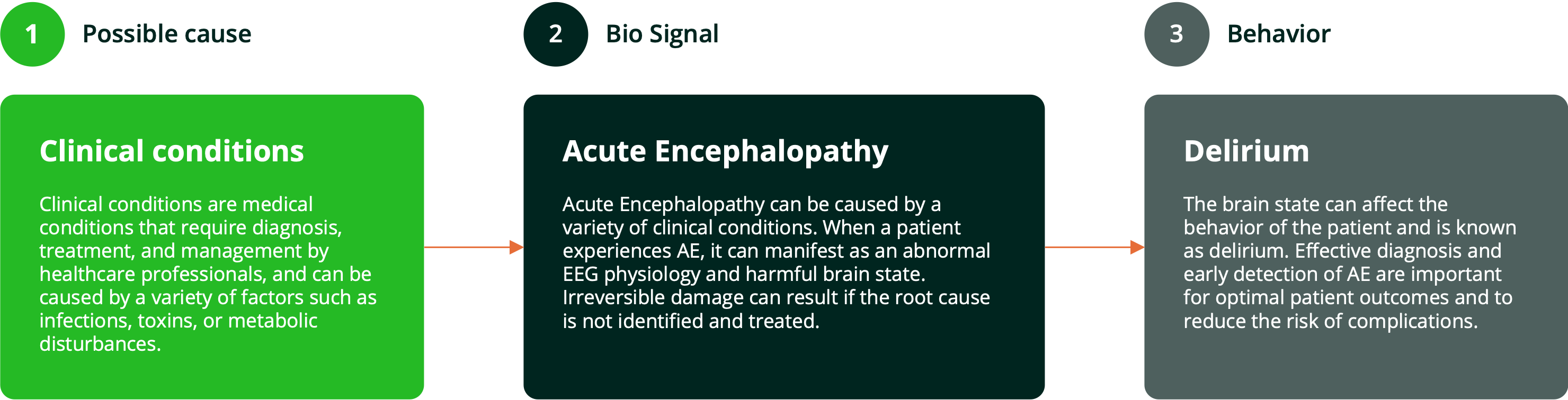
Acute Encephalopathy (AE) is a harmful brain state, often affecting patients in clinical conditions and characterized by abnormal EEG physiology. When AE affects the behavior of the patient, it is known as delirium ( ). Studies have shown that up to 40% of patients in post-surgical floors or ICU are affected by acute encephalopathy (
). Studies have shown that up to 40% of patients in post-surgical floors or ICU are affected by acute encephalopathy (
 ).
).
Frequently asked questions
Acute encephalopathy and delirium
What is acute encephalopathy?
What is delirium?
Delirium is also called acute confusion or acute brain failure. This confusion develops in a short time (usually within a number of hours or days), can fluctuate in severity during the day and always has a physical cause (American Psychiatric Association – Diagnostic and Statistical Manual of Mental disorders, Fifth Edition, DSM-5). Delirium is diagnosed based on clinical characteristics.
What causes acute encephalopathy and or delirium?
Acute encephalopathy and delirium always have an underlying physical condition. In other words, the same condition (complication) causes and EEG response in the brain and can lead to behavioral changes. In this case, medically, we are looking at the same thing, or things, as the cause can be multi factorial.
What subtypes of acute encephalopathy exist?
What is the difference between a hyperactive and a hypoactive delirium?
Delirium can express itself in different types. Up to 75% of delirious patients have hypoactive or silent delirium. With the current screening instruments, this group is often missed. Only 12% to 35% of delirious patients are recognized (Marcantonio, 2017, NEJM).
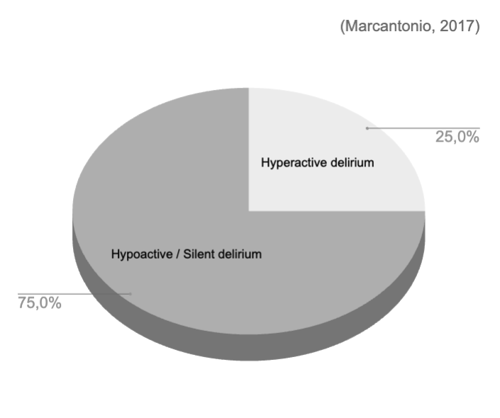
- Hyperactive type: Patients with hyperactive delirium are restless, often agitated, and exhibit physical hyperactivity.
- Hypoactive type: Patients with hypoactive delirium are calm and may appear sleepy. This type is often mixed up with depression or dementia.
- Mixed type: Patients with this type are occasionally restless.
Hypoactive (silent) delirium is more difficult to recognize than hyperactive delirium and can often be confused with dementia or depression. Because of this lack of recognition, hypoactive delirium has been associated with worse patient outcomes.
Who can develop acute encephalopathy and delirium?
Anyone can get acute encephalopathy / delirium. Older age, vulnerability (permeable blood-brain barrier) and dementia significantly increase the risk.
Why is it serious?
Every year, 20 million patients are at risk of AE/D in EU and US hospitals, which can lead to long-term cognitive impairment, extended hospital stays, and increased healthcare costs.
Acutely, severe encephalopathy may lead to loss of consciousness or coma. Some encephalopathies can be fatal.
People with delirium usually don’t know they’re confused themselves. Delirium is very scary for patients and their family and sometimes make providing care in hospitals more challenging. The confusion usually decreases as the physical condition improves. The period of confusion varies from a few hours to weeks. Not all patients fully recover from delirium. Many patients keep residual symptoms, such as memory and concentration disorders, for a longer period of time.
How is can it be treated?
The most important thing is to address the underlying disease(s) or cause(s) as soon as possible. The causes of encephalopathy are numerous and varied. Examples of steps to take are:
- Investigate a disturbance in the electrolytes
- Look for an emerging infection or sepsis
- Assess the (accumulation of ) medication
- Perform X-thorax to check for lung infections
- Et cetera
- The use of glasses and/or hearing aids;
- Reassuring and helping to orient the patient, and avoiding conflicts;
- Early mobilisation: helping the patient to get out of bed and get up;
- Let the patient sleep peacefully at night;
- Talk quietly and play games or puzzles together with the patient.
Interested? Let's get in touch!
Get in touch to learn how you can reshape acute encephalopathy and delirium care delivery
pageversion: 3.0

