What is acute encephalopathy and what is delirium?
- Knowledge base
- Acute Encephalopathy & Delirium

Acute encephalopathy & delirium
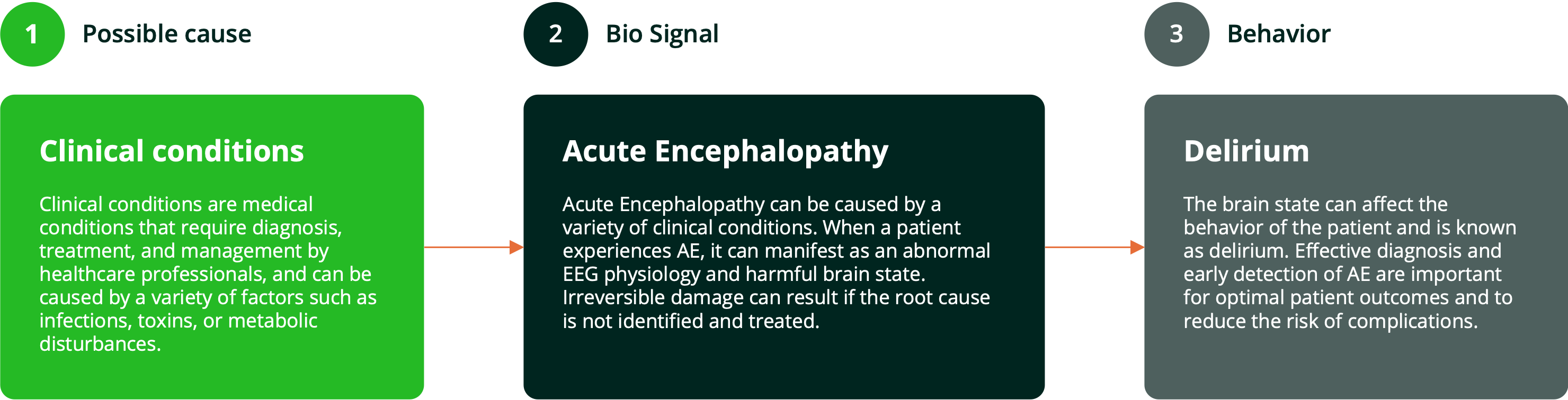
Acute encephalopathy often manifests itself as delirium. Delirium is diagnosed based on clinical features. Both diagnoses are characterized by an underlying cause.
Research shows that only 12% to 35% of delirious patients are recognized with current screening tools (
 ).
).
Better detection is key
Acute encephalopathy and delirium are always associated with an underlying condition. Use of an objective bio signal enables more timely diagnosis and treatment of this underlying condition.

The impact of acute encephalopathy and delirium
A very frequent healthcare problem
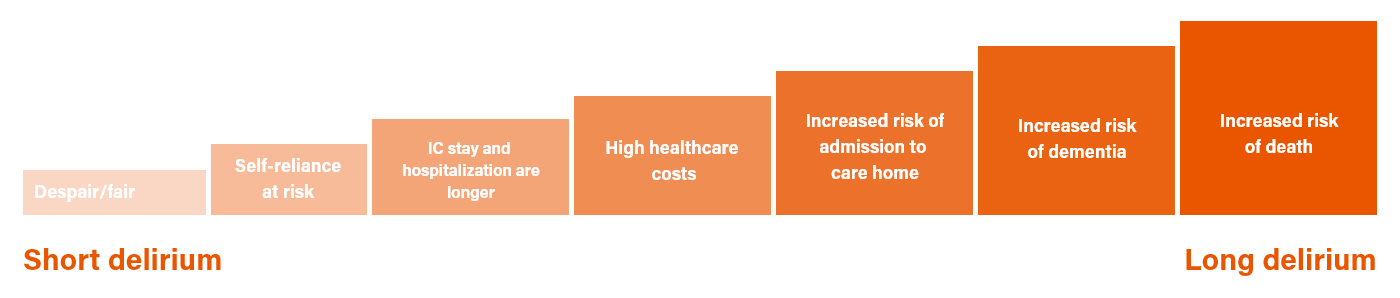
The longer delirium lasts, the higher the impact
Often recognised too little and too late
Within clinical practice, there is a need for better recognition of acute encephalopathy and delirium. Using questionnaires, the majority of patients are missed and often only patients with hyperactive delirium are recognized.
Current situation
Using checklists that are highly subjective and require symptoms to be present
Lack of certainty in evaluating clinical signs often leads to delayed diagnosis and treatment
Only 12-35% ¹ of delirious patients are recognized with current screening tools
Acute encephalopathy is by definition missed because EEG is the only method to detect.
Uncertainty about patient’s brain state using subjective tools does not allow staff to direct care to those in need
Dependent on precious nursing time for qualitative assessment
With our program
Objective screening protocol allows risk stratification for clinicians providing better deployment of precious nursing resources
Early, objective assessment of brain state ²
Provides clear five-point scale to trigger investigation of underlying conditions
Diagnostic performance > 85% for acute encephalopathy
Easily assesses normalization of the brain state when treatment is applied
Interested? Let's get in touch!
Get in touch to learn how you can reshape acute encephalopathy and delirium care delivery
sources: ¹ Marcantonio, et al. N Engl J Med, 2017; ² Ditzel, F.L., et al. Psychiatry Clin Neurosci, 2022
pageversion: 3.0







